1. WHAT is Malnutrition
Malnutrition is a broad term that refers to both undernutrition and overnutrition. Undernutrition has 4 broad sub-forms namely: wasting, stunting, underweight, and micronutrient deficiencies. Overnutrition is characterized by being overweight and is often because of poor dietary habits and sedentary lifestyles. The three types of undernutrition that are specifically significant in emergencies situation are.
- Acute malnutrition is directly due to illness or inadequate consumption of food, or nutritional oedema.
- Chronic malnutrition is characterised by stunting (inhibited growth in height and cognitive development caused by poor nutrition over a period)
- Micronutrient deficiencies is due to sub-optimal intake of one or more essential micronutrient.
Acute Malnutrition
There are 2 sub-groups of acute malnutrition amongst children; Moderate Acute Malnutrition (MAM) which is defined as weight-for-height (WFH) of less than 2 standard deviations (SD) of the reference population median weight-for height or less than 125 cm Mid Upper Arm Circumference (MUAC). The other form of acute malnutrition is Severe Acute Malnutrition (SAM) which is defined as a weight-for-height of less than 3 standard deviations or less than 115cm MUAC, or bilateral pitting Oedema. Severe Acute Malnutrition (SAM) is further subdivided into 2 forms: Marasmus and Kwashiorkor. Marasmus is defined by the severe loss of body fat and muscle and Kwashiorkor by the presence of bilateral pitting oedema of both feet. Children who have kwashiorkor may not appear underweight initially because of their Oedema, hence Oedema is a separate criterion for admitting children with SAM into nutrition programs and is not measured by WFH or MUAC measurements but rather assessed through clinical signs as shown below. Therefore MUAC, weight-for-height, and bilateral oedema are all independent criteria for admission to treatment programmes, meaning that only one criterion needs to be met to be eligible for treatment. There is currently no consensus on how to identify pregnant women as acutely malnourished and when to enrol them in nutritional programmes. However according to the SPHERE Guidelines, MUAC may be used as tool to screen for malnutrition in pregnant and lactating women and as a criterion for entry into a feeding programme. The guidelines states that cut-off points for risk vary by country and range from 21 cm to 23 cm. For more information on anthropometric assessment see Annex 5.1.
| Types of Acute malnutrition | Clinical signs and anthropometric cut offs |
| Moderate acute Malnutrition in children | Moderately wasted, with WFH below 2 SD or MUAC of less than 125 mm. |
| Marasmus (Severe acute Malnutrition) in children | Extreme wasting, little fat or muscle, child’s skeleton clearly visible, lack of appetite in complicated cases with WFH less than 3 SD or MUAC of less than 115mm. |
| Kwashiorkor (Severe acute malnutrition) in Children | Bilateral Oedema of both feet; thin, sparse and pale hair that falls out easily, dry scaly skin especially on the arms and legs, a puffy or moon face and apathy. |
| Moderate Acute Malnutrition in pregnant and lactating women (PLW) | Moderately wasted, with MUAC of less than 210 mm or 230mm. |
Chronic Malnutrition
Chronic malnutrition is characterized by stunting (short stature for age) which is defined by inhibited growth in height and cognitive development. It is measured by low height-for-age of less than 2 standard deviations (SD) of the WHO reference population median height-for age. Stunting is the result of chronic or recurrent undernutrition due to poor socioeconomic conditions, poor maternal health and nutrition, frequent illness, and inappropriate infant and young child feeding and care in early life. It develops within the first 1,000 days of life (from conception to the age of two) and results in irreversible stunting of both cognitive and physical development. Thus, maternal nutritional status before and during pregnancy is very important and are determining factor of child nutrition.
Micronutrient Deficiencies
Micronutrients are vitamins and minerals needed by the body in very small amounts. Micronutrient deficiencies (MNDs), like all forms of undernutrition, occur due to insufficient intake and/or impaired absorption due to infection, disease, or inflammation. During emergencies, access to diverse foods is often a great challenge and a major cause of MNDs. Micronutrients of public health significance include iron, iodine, Vitamin A, Vitamin C, Zinc and folate as they cause widespread global micronutrient deficiencies especially in pregnant women and their children under 5 years who are the highest risk. MNDs are often referred to as hidden hunger and is often difficult to confirm clinically in emergency settings as biomarkers are not practical or feasible for widespread assessment outside of the clinical setting. Therefore, in the absence of diatary or biomarker data, we can only assume that countries with a high burden of undernutrition also have a high burden of MNDs[1].
Causes of Acute Malnutrition
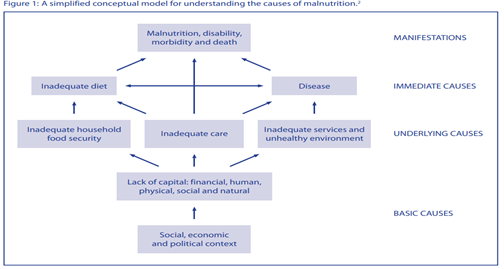
The different causes of malnutrition are best explained by the UNICEF’s 1990 conceptual framework of malnutrition, which since then have been adapted several times (see Annex 5.2). The IPC acute malnutrition classification system also uses this analytical framework for analysis. Through this framework, we can analyse the different causes of malnutrition (which is the outcome or manifestation) by understanding the immediate, underlying, and basic causes of malnutrition. The immediate causes of malnutrition are inadequate dietary intake and disease. Inadequate dietary intake and diseases are caused by food insecurity, inadequate care for women and children, insufficient health services, and unsanitary environments. Therefore, it’s important to understand the food security situation, caring practices (including infant and young child feeding), access to maternal and child health services and WASH in an emergency when determining the likely impact on malnutrition. For example, open defecation and inappropriate hygiene and sanitation practices, especially during an emergency can increase the spread of infectious diseases such as acute water diarrhoea, scabies, measles, malaria etc. Infection increases the body’s requirements for nutrients, reduces appetite, and affects the absorption of nutrients from the gut, which leads to malnutrition. While infection can cause malnutrition, vice versa is also true as malnutrition can increase the risk of infection setting up a vicious cycle. A malnourished child, whose resistance to illness is poor, falls ill and becomes more malnourished, which reduces his capacity to fight against illness and so on.
The basic causes of malnutrition include political, economic, legal, and ideological factors (including religion, culture, and tradition) which may prevent from attaining good nutrition. For example, these include the extent of which rights of women and girls are protected by law; the control they have over resources; the political and economic systems that determine how income and assets are distributed; and the policies that govern social sectors. The physical environment people live in can also play a role. For example, areas with frequent droughts, unreliable rainfall, flood prone, intense heat also impact on nutrition status. Political discrimination due to religion, race or clan can lead also to systematic marginalisation and exclusion from food and other available relief services and is one of the basic causes of malnutrition. In emergencies such groups may be too afraid to seek assistance or are ignored by the decision makers. In summary, the conceptual model highlights that malnutrition is not caused just by insufficient food intake. It demonstrates the complexity of connected factors that impact on nutrition at different levels hence any nutrition analysis must be take all these factors into account during an emergency.
What is a nutrition emergency?
Access to food and adequate nutritional status are critical determinants of people’s survival in a disaster. Malnutrition in its various forms often emerge during emergency situations, both natural and man-made ones when access to sufficient, nutritious food, health services, clean water and care and hygiene practices are compromised. In such situations there is an escalation of communicable diseases and most notably the big five diseases that are most severe amongst children under five years of age, i.e., measles; diarrhea; malaria; respiratory infections and malnutrition. During emergencies, even being mildly underweight is associated with increased mortality. WHO estimates that malnutrition is an underlying cause in almost half of all under-five child deaths[2]. The biggest killer in emergencies is child malnutrition that is either recorded as a direct or as an underlying cause of death. When classifying a nutrition emergency, it’s recommended to consider the overall trend in in global acute malnutrition (GAM) and Severe Acute Malnutrition (SAM), often a GAM of >15% or 10-14% with aggravating factors is considered to warrant an emergency nutrition response. However, it is important to not wait until a certain threshold has been reached before deciding to intervene as preventing malnutrition and its associated mortality is very important in an emergency. In addition, in certain contexts you need to consider additional risk factors such as prevailing high micronutrient deficiencies, childhood morbidity or doubling of GAM rates in short period of time even if in terms of absolute number, the prevalence is “low”, e.g., below 10%. In a nutrition emergency where the prevalence of acute malnutrition among young children might be 10% to 15% and of severe malnutrition, 2% to 3%, mortality rates can be very high. Elevated crude mortality and under-five mortality rates are also benchmarks for and definitions of a nutrition emergency. The Global Nutrition Cluster decision tool for emergencies for Moderate acute Malnutrition (Annex 5.3) can help you choose the most appropriate responses to address MAM in a particular emergency setting.
Who are most nutritionally vulnerable in emergencies?
Protecting the nutritional status of vulnerable groups affected by emergencies is important and a basic humanitarian right. The population groups most nutritionally vulnerable in emergencies can be categorised according to their:
- Physiological vulnerability (e.g., young children, pregnant and lactating women, older people, disabled, and people living with chronic illness such as HIV and AIDS)
- Geographical vulnerability (e.g., people living in drought- or flood-prone areas or in areas of conflict)
- Political vulnerability (e.g., oppressed populations)
- Internal displacement and refugee status (e.g., those who have fled with few resources and livelihoods)
Classifying Malnutrition
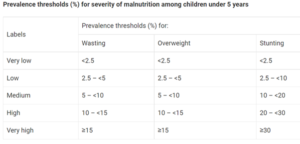
There are new prevalence thresholds for classifying the severity of different forms of malnutrition which has been established through the WHO-UNICEF Technical Advisory Group on Nutrition Monitoring (TEAM)[1]; it is recommended that these new thresholds will replace the current WHO ones that have been in place for a long time[2]. The thresholds were developed in relation to standard deviations (SD) of the normative WHO Child Growth Standards. The international definition of ‘normal’ (two SD from the WHO standards median) defines the first threshold, which includes 2.3% of the area under the normalized distribution. Multipliers of this “very low” level (rounded to 2.5%) set the basis to establish the subsequent thresholds. For more information kindly refer to Annex 5.1.
Nutrition Assessment
Nutrition assessment involves taking anthropometric measurements (measuring parts of the human body) and collecting information about an individual’s clinical and biochemical characteristics, dietary practices.
Why is nutrition assessment important?
- To identify people at risk of malnutrition for early intervention or referral before they become malnourished.
- To identify malnourished individuals for treatment
- To track child growth.
- To identify medical complications that affect the body’s ability to digest food and utilize nutrients
- To detect practices that can increase the risk of malnutrition and infection
- To inform nutrition education and counselling
- To establish appropriate nutrition care plans
Nutrition Assessments Methods
Nutritional assessment can be done using the ABCD methods:
- A. Anthropometry
- B. Biochemical/biophysical methods
- C. Clinical methods
- D. Dietary methods
The target population of nutrition surveys and interventions during emergencies are mostly children aged 6-59 months old, pregnant, and lactating women. However, there are also international standards for measuring malnutrition in adults, older children, adolescents, and the elderly. The most common emergency indicators collected during a nutrition survey are:
- Global Acute Malnutrition (GAM) – weight-for-height z-score <-2 and/or oedema,
- Severe Acute Malnutrition (SAM) – weight-for-height z-score <-3 and/or oedema,
- Oedema (bilateral Pitting oedema)
Mid upper arm Circumstances (MUAC) and Weight for Height (WHZ) are the anthropometric measurements taken to identify children most in need of treatment for acute malnutrition recommended by WHO. Bilateral pitting oedema is also a clinical method of diagnosing severe malnutrition on its own, regardless of the results of anthropometric assessment. MUAC is commonly used in the community to identify and refer children 6−59 months of age with acute malnutrition, it is also used to conduct mass screening as its easier to do within the community compared to taken weight and height of every child, in insecure areas with limited access and as a temporary programming adaptation to COVID-19 where Infection Protection Control (IPC) measures cannot be assured. However, MUAC, WHZ and Oedema can be used in health facilities to diagnose children with acute malnutrition and enroll them into treatment. In terms of program implementation WHO recommends using any of the three indicators to identify acute malnutrition, but one must use the same indicator for both diagnosis and discharging children out of treatment programs. Both MUAC and WHZ have their strengths and weaknesses and evidence suggest that MUAC is good at predicting the risk of death in children with SAM and selects younger children at highest risk while WHZ has tendency to select older children. Hence since both indicators choose different sub-groups of children and there is a great overlap between the two the GNC recommends the use of all the indicators for the assessment and treatment of acute malnutrition, including all children with low MUAC, low WHZ or bilateral pitting oedema – known as combined GAM (cGAM).
For Surveys Weight-for-height is used as the main indicator of malnutrition. It is robust, independent of age for children, has an internationally accepted reference population, and its interpretation is based on wide experience in many parts of the world. Boys and girls are treated separately; however, it is recommended that MUAC measurement be included in all anthropometric surveys and that the two criteria are not alternative measures of the loss of body tissue, but complementary to one another thus should both be used independently to guide admission for treatment of malnourished children[1].
Dietary assessments are conducted to understand the quality and quantity of the diets consumed and it’s often done using the following methods.
- 24-hour recall methods
- Food frequency questionnaire
- Food group questionnaire
This is useful especially when designing nutrition interventions aimed at improving dietary diversity, quantity and quality through social behavior change communication (SBCC) or cash for nutrition outcome.
Biochemical assessment is often not done during emergencies as it’s often not practical to check the levels of nutrients in a person’s blood, urine, or stools due to lack of lab facilities and tools needed. Also, this can only be done by medical professionals, but this method obviously can give more useful information about the medical problems that may affect appetite or nutritional status.
For further information on nutritional assessment using different methods please see Annex 5.4.
When should you conduct a Nutrition survey?
- To establish baseline data to determine if a nutrition emergency exists
- To estimate the severity and geographical spread of a nutrition emergency, including the groups most affected or at risk.
- To assess the likely impact of the emergency on health and nutrition because of primary drivers of malnutrition.
- To determine the need or expand existing nutrition interventions
- To determine the effectiveness of nutrition programs.
- To determine the need to establish or expand nutrition surveillance
What are the key factors to consider when planning a nutrition survey?
- Determine the relevance and timing of doing a survey
- Gather existing and contextual information from local partners and authorities
- Define survey objectives
- Define the geographic area and population group(s) to be surveyed
- Decide what additional information to collect.
Conducting a nutrition survey is expensive and time-consuming, therefore before starting an assessment you should ask the following questions:
- Are the needs of the affected population obvious? If yes, then implementation takes priority over a survey and hence can be deferred.
- Are the results critical for decision making?
- Has anyone else done a SMART survey in the areas recently? If yes use their data.
- Will it be possible to implement evidence-based recommendations? There is little point in doing a survey if it is already known that a response will not be possible
- Is the affected population accessible? Insecurity or geographical constraints may result in limited access to the population of interest. If this is extreme, a survey cannot be conducted.
Seasonal changes in malnutrition exists, for example in a context where seasonal cycles might have a serious effect on household’s food security, surveys should be conducted at periods of highest or lowest nutrition and food security risk, i.e., harvest time or hunger gap. Also, during the rainy season where the risk of water-borne diseases is higher the effect of seasonality might be observed in increases in admissions to feeding centers hence this is also indicative of seasonal effects.
Where can I find important manuals on how to design and analyze nutrition surveys?
To conduct a cross-sectional representative nutrition survey, you should always follow the SMART methodology which can be used for both a rapid and a full assessment. This will require a SMART manager’s training and certification, alternatively the country office can hire a SMART Survey consultant to do this. Below are the resources available on survey designs and methods.
- SMART (2017) Measuring Mortality, Nutritional Status, and Food Security in Crisis Situations: SMART Methodology. SMART Manual Version 2 published in 2017. Available for downloaded here
- CDC/WFP (2005) A Manual: Measuring and Interpreting Malnutrition and Mortality. Available here
- Duffield A, Taylor A (2004) Emergency Nutrition Assessment: Guidelines for Field Workers. Save the Children. Available here
How to do a Nutrition Situation Analysis?
A nutrition situation analysis helps you to define and categorize the severity of a given humanitarian situation across geographical areas based on the magnitude of the nutritional needs of the population. There is a list of core nutrition indicators and thresholds for acute malnutrition and its contributing factors that have been developed by the Global Nutrition Cluster (GNC) taskforce to streamline nutrition situation analysis. These indicators are aligned with the IPC AMN (acute malnutrition) analytic framework. This will provide you with a common approach for classifying the severity of malnutrition and identifying its key drivers in your country, it will also allow decision makers the ability to compare across context between one area or country to another. The core list of nutrition indicators and contributing factors with thresholds can be found in Annex 5.5. In a situation where the GAM in your country is above 5% and there is an IPC AMN analysis done at country level then you can use that data for your nutrition situation analysis, however you must ensure the validity period of the existing IPC AMN severity classification. If the situation has significantly changed, then there is a need to update the analysis in consultation with the IPC country taskforce and in consultation with your nutrition cluster.
[1] Grellety and Golden BMC Nutrition (2016) 2:10. Available online
Estimating Nutrition Program Caseload
In any nutrition response that includes management of acute malnutrition in children under 5 years, pregnant and lactating women (PLW), it is important to accurately estimate the number of children and PLWs to be targeted for treatment services. Without being able to do this right you risk either over or underestimating the target beneficiaries, which can have huge program implications, especially when it comes to estimating the supplies needed and resources. The total number of children under 5 and PLW needing treatment services during the project cycle can be achieved by either using a caseload calculator (see Annex 5.6) or you can do this manually. To calculate the total number of children or PLW with Acute Malnutrition (AM) to be targeted by the project, follow the steps below.
- The total burden of AM = existing cases + new cases
The existing cases are those currently malnourished and can be obtained by multiplying AM prevalence rate with the number of children aged 6 to 59 months in the population.AM prevalence x number of children under five in the populationsThe prevalence rate of acute malnutrition, also termed GAM, can be obtained from recent SMART surveys, if there is no SMART data then proxy GAM can be used from mass screening data. The proportion of children under 5 years, pregnant and lactating women (PLW) in the population can be obtained by census, demographic surveys, and SMART surveys. Once you know the proportion of children under 5 and PLW in the population, you multiply it with total population estimate data to obtain the number of children and PLW in that population.For example: if 20% of the population are children aged 6-59 months and the population size is 18,000 then the expected number of children aged 6-59 months is 3,600 (20% x 18,000)The New cases are those expected to be malnourished during the project, so this is looking at new incidences of malnutrition during the project period and those currently expected to be malnourished. To do this a general rule of thumb is to use what is called the incidence correction Factor (K). For short term emergency projects that last between 3-6 months, an incidence correction factor of 1.6 is generally used and for projects between 8-12 months K of 2.6 is used.However according to more recent studies on incidence of malnutrition and the actual burden of acute malnutrition, it is advised that a more contextualized incidence data should be used whenever possible in countries where incidence of malnutrition is known to accurately estimate the burden of acute malnutrition. Hence check with your local nutrition cluster team if you are unsure of what incidence rate is used in your country.Once you have decided on the incidence rate to use you can sufficiently estimate the total burden of acute malnutrition by using the formula below. - AM prevalence x number of children aged 6-59 months x KOnce you get the total cases of malnutrition in the area, then the final thing to decide on is the coverage. According to SPHERE standards, coverage in rural areas should be more than 50%, in urban areas more than 70% and in camp situations more than 90%.In Summary the formula for estimating nutrition caseloads or target for treatment programs are. The same formula can be applied to get target Caseload for PLWs and for MAM treatment program.
Formulae: P x N x K x C
P = Prevalence of acute malnutrition
N = Number of children or PLW in the affected population
K = Incidence correction Factor
C = Targeted program coverage
TIP 1: If SAM prevalence is not known, consider using on average an estimate of 20% of GAM to be suffering from SAM; and 10% of the SAM cases have medical complication and need impatient care.
Example Calculations
We want to estimate the total number of children aged 6 to 59 months suffering from Severe Acute Malnutrition (SAM) without medical complications who will be targeted and admitted in an OTP (Outpatient Therapeutic program). From the national census we know that the total number of children aged 6 to 59 months is 20% of the population. In X town there are 86,000 people, hence, the total number of children under 5 living in this town is 17,200. SAM prevalence is 1.8% according to a recent SMART survey in that area. The program is planned in rural areas, so we agreed to apply a coverage of 50%.
Total target of SAM children aged 6- 59 months will be = 17,200 x 1.8% x 2.6 x 50% = 402
We agreed that on average 90% of the SAM cases detected will be admitted in OTPs and 10% admitted in Stabilization center (SC) therefore this project will target 90% of 402 (361) for the OTP services.
[1] Bailey R.L., West Jr. K.P., Black R.E. The Epidemiology of Global Micronutrient Deficiencies. Ann Nutr Metab 2015;66(suppl 2):22-33.
[2] https://www.who.int/news-room/fact-sheets/detail/malnutrition, accessed 11th April 2022.
[3] WHO. UNICEF New Prevalence Thresholds for Stunting, Wasting and Overweight in Children. [(accessed on 22 March 2021)]; 2018 Available online
[4] De Onis, M., et al. (2018). Prevalence thresholds for wasting, overweight and stunting in children under 5 years. Public health nutrition, 22(1), 175–179.